A team of champions: Dean’s unexpected battle with COVID-19

Within just 14 days, Dean Goranson went from being healthy with no underlying health concerns to being intubated in the Intensive Care Unit after testing positive for COVID-19 two weeks prior.
Dean monitored his health while in quarantine with his wife and two teenage boys. During quarantine, Dean was experiencing the typical COVID symptoms of a fever, chills, and a headache, but it wasn’t until the fourteenth day of quarantine during breakfast that Dean’s breathing became quite laboured.
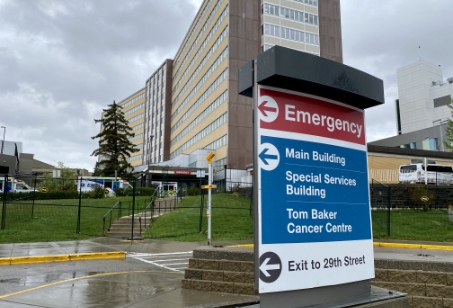
Dean’s wife, Jeanine, dropped him off at the Emergency Department expecting to see him in a few short hours after receiving some oxygen support.
She was blindsided when a call from the hospital left her with crippling uncertainty whether she would ever get to hug Dean or hold his hand one more time. It was two weeks before she and her boys got to wrap their arms around him again.
After being told by the ICU team that if he were not put on a ventilator, he would die, Dean said, “Do whatever you have to do; I’m not going to die and I don’t want to die.” These are the last words that Dean remembers saying to his care team prior to being intubated on a ventilator for five days.
Within 18 hours after admittance, Dean’s breathing was so laboured that he was transferred to the critical care of the Intensive Care Unit (ICU) team, and later the COVID unit, where they cared for more than just Dean’s frail condition.
Not being able to be by his side, Jeanine and their boys worried constantly about his condition. Beyond caring for Dean’s physical needs as he fought against the virus’ attack on his body, the care team in the ICU became the family’s champions, supporting Dean and bringing Jeanine along for every step in his recovery. They understood how important Dean’s family was to his wellbeing, and were diligent in ensuring Jeanine and the boys were connected and up to date on his condition, despite being unable to visit him in person.
Two weeks later, Dean walked out the doors of the hospital and into the front door of his home.

We could not let the compassion and love of Dean’s care team go unnoticed. If it wasn’t for them, and the support they gave to me and my boys during this grave time, we wouldn’t have Dean with us here today.
Jeanine goranson
The increased demand on ICU care
Foothills Medical Centre
admitted
During 2020, the Foothills Hospital ICU admitted to their unit over 1,300 patients and has been instrumental in the care of the most critically-ill.
Foothills Medical Centre has been critical in the care for some of the sickest COVID patients with staff feeling the burden of the high rates of hospitalizations, especially during wave two and wave three.
During 2020, the Foothills Hospital ICU admitted to their unit over 1,300 patients, and large-scale surge plans were developed to increase the site’s ICU capacity from 30 to 150 beds demonstrating the high demand and showcasing the strategic problem-solving skills that staff face on a daily basis.
Peter Lougheed Centre
admitted
Thru the COVID-19 pandemic, Peter Lougheed Centre’s ICU expanded to 27 beds, caring for nearly 800 patients.
The Peter Lougheed Centre’s ICU is the second largest in the Calgary zone. In 2020 the intensive care team cared for nearly 800 patients. Through the COVID-19 pandemic, Peter Lougheed Centre’s ICU expanded to 27 beds, cohorting in several of the rooms and overflowing into the CCU at times.
The hospital admitted 42% of all COVID-19 patients within the Calgary zone. The facility was also home to the only field hospital location in Calgary, which gave the site the flexibility they needed to ensure controlled isolation spaces for patients with COVID-19.
Rockyview General Hospital
admitted each year
Approximately 475 patients who need critical care and life support are admitted to Rockyview General Hospital ICU each year.
Over the past 18 months, Rockyview served as an important support for the other hospitals and ICUs across the city, consistently operating at overcapacity during peak waves. Rockyview General Hospital is part of a coordinated pandemic response to ensure all COVID and non-COVID critically ill patients receive the care they require.
South Health Campus
critically-ill patients
In support of the pandemic response, South Health Campus shifted to focus on care for COVID positive patients and adapted its ICU from ten beds plus two CCU beds, to 16 dedicated spaces for the most critically-ill.
To ensure that ongoing care was unwaivering during the peak waves of the pandemic, the teams planned for expansion of care for COVID-19 and anticipated ICU patients to allow for care of up to 95 patients.
 Spotlight
Spotlight
Donor gives a life-saving advantage in preparing for COVID-19 critical care
A gift from Rotary Club of Calgary North just prior to the COVID-19 pandemic had exponential impact in ways that no one could have anticipated. Thanks to their generous support, the Extracorporeal Life Support (ECLS) team at Foothills Medical Centre purchased a Parallel Simulator, a state-of-the-art training system that is customizable and portable so that it can be used in a variety of ways. Able to simulate numerous scenarios, this important piece of technology helped prepare teams for the increasing complexities of patients requiring life support due to COVID-19.
Extracorporeal Life Support (ECLS) is a technique that allows clinicians to provide prolonged cardiac and respiratory support. ECLS has become the standard for this type care and can be used on people of all ages ranging from neonates to adults. Patients needing ECLS often experience situations in which their heart and/or lungs are not able to sustain life on their own. Some forms of life support assist heart and lung function so that it can continue for short periods of time to facilitate operations like open heart surgery. ECLS, on the other hand, can last for weeks if necessary.
Often ECLS is used on patients with the following conditions:
- When patients with lung or heart disease become critically ill and are candidates for a transplant;
- In situations where a patient’s lungs are not able to provide enough oxygen to the body;
- When a patient’s lungs cannot get rid of carbon dioxide even with assistance;
- When the heart is unable to pump enough blood to the body.
How your support advanced COVID-19 care
It’s been a year… But because of your generous support for COVID-19 response and recovery we’re making it through! Thank you for being an important part of the support needed to keep going through this challenging year.
related initiatives
Your support has rallied our health care workers on the frontlines.
Breakthrough investments made in COVID-19

COVID-19 spotlight: rallying our front-line workers
During the holidays, when hospital rates were surging, donors shared the spirit of giving and appreciation through the Feed the Frontline campaign.
Your generosity resulted in providing 22,000 health care workers with Sunterra-supplied meals. It was a chance for the community to say ‘thank you’ and for our front-line workers to have some time to rejuvenate and fuel for their next shift.

I have worked for over 14 years as an RN and this has been the most heartfelt and rewarding gesture I have ever received as a frontline worker. I cannot underestimate the impact a simple "Thank you" from a family or that a patient brings, however, the kindness and thought that donors have put into this is overwhelming.
Caroline Lowther RN, BN


Stories of Impact
Your support of Calgary Health Foundation has funded breakthroughs that are transforming lives. See how!



 Read Story
Read Story Covid-19 Impact
Covid-19 Impact