2022 Impact Report
Looking forward:
Mental Health
Supporting the urgent need for mental health and addictions treatment breakthroughs
150,000 Calgarians require addictions and mental health support

Mental health and addiction challenges may be largely invisible illnesses – but their impact on individuals, families and the health care system are significant and critically need our support. In partnership with a wide range of organizations, we are dedicated to working towards breakthroughs in care, wellness and research that will transform the lives of countless Albertans.
Unlike many issues people may face with their health, substance use disorders and mental health presents unique challenges. From the cascading effect these issues have on families and communities to the social stigmas and other barriers that get in the way of critical treatment, equally unique solutions are required – and urgently. There’s no single solution – but a continuum of care and inclusive consensus of all stakeholders are paramount.

Valuing voices
True progress with substance use disorders and mental health care is only possible by listening deeply to the lived experiences of those with experiences suffering first and second hand and the health care staff on the front line.
We’ve worked hard with the City of Calgary, Alberta Health Services (AHS) and the University of Calgary to create open dialogue between researchers, practitioners, survivors, people experiencing mental health and addiction illnesses and their families and communities to discover the true barriers and challenges – and develop the short- and long-term strategies that will break through barriers in receiving the right care at the right time.

It’s like being in a jail cell. You know, I’m getting worse, I feel worse, I feel more depressed I feel...
CALGARY EMERGENCY ROOM PATIENT
A continuum of care
There’s no single solution – but a continuum of care and inclusive consensus of all stakeholders are paramount.
Both in society and the health care system, mental health and substance use issues only become visible at crisis points.
Whether it’s how they manifest themselves disproportionately among people experiencing homelessness, the justice system or the emergency room, hospital intervention in these times of crisis have traditionally been the primary focus.
A focus on the full continuum of care is necessary to empower breakthroughs in the lives of people affected most strongly by these illnesses. While crisis care intervention is paramount, an enhanced focus on prevention support and short- and long-term support for patients returning to their communities after treatment will transform lives. While our hospitals must be equipped and prepared to care for patients in their darkest and most vulnerable moments, we must also ensure that our health care system is empowered to provide patients and their families with a pathway and necessary support to help individuals manage their illnesses at home and in the community.
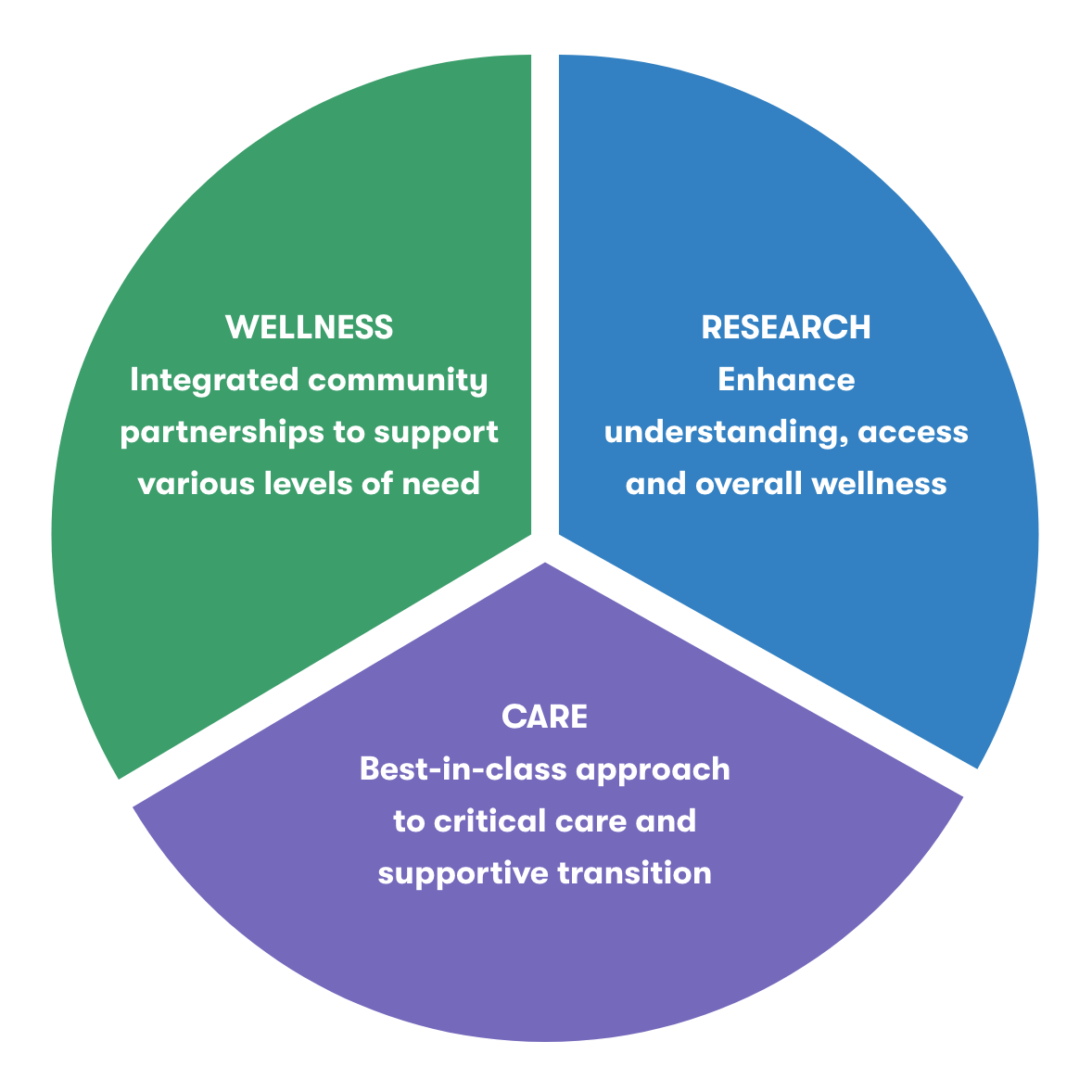
Focus on Wellness:
Partnership with community agencies and mental health experts to ensure the right care at the right time at the right place.
Focus on Research:
Over $2.5M in funding committed to research that enhances our understanding of key challenges in mental wellbeing, reduces stigma in care and creates better support systems for vulnerable citizens.
Focus on Care:
Enhancing critical care access with a trauma informed approach to space design and care in hospital emergency departments and short-term stay units. Establishing a better model for transition support from critical care environments to community-based services, closing the gaps for continuous care.
$500M
in costs to Calgary's Health Care system
30%
of Canadians will experience mental illness or a substance misuse disorder
50-90%
of people with police contact have addictions and mental health challenges
4X
more likely to be arrested
Five Areas of Focus
Through an integrated process of research and stakeholder consultations, a handful of primary themes of need have become extremely clear:
01
Trauma informed space design in hospitals needs to be an investment
02
Mental health peer support and patient advocacy in hospitals is critical
03
Stronger support networks are needed for patients transitioning to community care
04
Investment in research and innovation will continue to evolve care
05
More supports are critical for frontline staff to treat mental health and addictions issues in tandem with other urgent issues
Every breakthrough has a beginning
After extensive engagement research and collaboration, the generosity of our donors is already making an impact through a selection of important investments.

Renfrew recovery centre triage vestibule
As Calgary’s only medical detox centre, the Renfrew Recovery Centre provides an invaluable breakthrough moment for up to 40 patients at any given time taking their first steps towards recovery.
Before COVID, the centre’s triage vestibule could hold up to 15 people waiting for treatment – but with pandemic safety measures in place the space could only accommodate eight at a time. With less space, patients seeking help were forced to wait in the parking lot or community – where they were forced to endure the cold weather and often reverted to harmful activities.
Through the generosity of our donors, we were able to support the Renfrew Recovery Centre with an extention that serves as an addition to their triage room which increases the access and enhances the safety for people seeking treatment.
Transforming spaces with trauma informed treatment environments
When seeking acute care for substance use and mental health issues, patients too often find themselves in spaces that unintentionally make things worse for them. Much of our hospital infrastructure was designed with pure utility in mind – but when working with patients with complex mental health challenges, a different approach is required: trauma informed design.
Trauma informed design is a unique approach to the creation of spaces patients spend time in, specifically known for reducing and removing known adverse stimuli and environmental stresses, actively engaging individuals in a dynamic, multisensory environment, supporting self-reliance, providing and promoting connection to the natural world, separating individuals from others who may be in distress, reinforcing a sense of personal identity and promoting the opportunity for choice while balancing program needs and the safety and comfort of the majority.
Working with the Peter Lougheed Centre, we supported the renovation of the emergency room mental health space, short-term mental health unit and psychiatric ICU into spaces through trauma informed design.

Primary research with a primary goal: tangibly improve outcomes
Behind every substance use and mental health crisis there are people: the patient, their family and community and the frontline staff providing treatment.
To better facilitate the breakthroughs each and every one of them so badly desires, a research project called EMBER (Exploring Mental health Barriers in Emergency Rooms) was mobilized.
The project conducted many interviews with everyone from patients to doctors and nurses to discover gaps in knowledge, training, care and understanding to make urgent changes in how treatment is provided and received and to address the damaging stigma that continues to surround it all.
Enhanced community supports where patients are at
For many patients, recovery from substance use disorders and mental health illnesses isn’t a one step process. Instead, it’s a breakthrough that comes with sustained effort and support.
To help empower care beyond the moments of hospital crisis care, two new pilot programs were created (and subsequently permanently funded): Recovery Coaches and Mobile Street Teams.
Recovery Coaches are people with personal lived experience with mental health issues and substance use disorders who are trained to help support and guide patients on their path towards recovery. These coaches provide support in numerous ways, ranging from motivational interviewing to presenting patients with resources and the help they may need to navigate the process and system.
Mobile Street Teams bring together Mobile Integrated Health Outreach Workers, Mobile Integrated Health City Center Team and Community Paramedics to help provide deeper care and access to resources for people facing challenges ranging from loss of housing to addictions and mental health. Once a patient is referred to the mobile street team, the team works collaboratively to build a plan for the patient and provide the support necessary to navigate the steps to execute it. By intervening early and before a person is in crisis and in need of hospital care, the mobile street teams aim to prevent severe outcomes and help provide breakthroughs earlier than ever.

Practical research in treating patients presenting with methamphetamine toxicity
Crisis calls for research with practical and punctual implementation required to impact patient outcomes.
With that in mind, we were excited to support a research project aiming to create a standardized program for treating patients with methamphetamine agitation in emergency rooms. Providing urgent care to a patient who is also experiencing methamphetamine-induced psychiatric concerns is an extremely challenging task – and one that has not been fully researched or formalized. While this effort only began in September of 2021, it’s already earned the attention of researchers and care providers across Canada and has the potential to create a path to important breakthroughs for countless patients

